 We wrote this explanation three years ago for a blog post before Idan’s 1st transplant. Thought I would repost this now for those following along. Also adding a link to explanation of Hyper IgM from the Hyper IgM Foundation site:
We wrote this explanation three years ago for a blog post before Idan’s 1st transplant. Thought I would repost this now for those following along. Also adding a link to explanation of Hyper IgM from the Hyper IgM Foundation site:
– So What Is a Bone Marrow Transplant (BMT)?
Currently, there is no way to fix the gene mutation that causes Hyper IGM, but there is a way of replacing the bone marrow and giving Idan a new immune system. One can look at the bone marrow as the army base that the immune system (as well as the blood) is created and trained in. The idea is, if Idan’s T-cells cannot produce the protein he needs, lets give him a new army base, with soldiers that know what they are doing. But it is not that simple:
1) Currently the army base in his body is filled with soldiers (even if they’re not too smart), so there is no vacancy for him to host someone else’s army.
2) Idan’s body (AKA, the equipment, building and land that needs protection) is a perfect match with his current army, and no other army (AKA the donor’s bone marrow) is going to know how to work it in the same way.
3) Any gap in the protection that his army is giving him (albeit a lazy one) will open up his body to infections.
4) In order to create a vacancy in his army base so that a new army can move in, the old one needs to be eliminated entirely. The way they do this is with chemotherapy, which has the nasty side effect of destroying the bone marrow, and in our case we want that. However, that process comes with its own risks of toxicity to the body.
With all the risks involved Amanda and I decided that BMT is the way to go. BMT will give Idan the best chance at a long and healthy life. We did a lot of homework and spoke to dozens of bone marrow teams around the world. We decided on Seattle because of the new type of chemo drug they are using (Treosulfan) that is less toxic than others. If all we need is to clear the army base from soldiers why bomb random cities and cause damage to the whole land?
– How will this cure Idan?
First they will use chemo and ATG to eliminate his bone marrow and suppress his immune system. This is what we are doing from Day -6 to Day -1. We then give Idan a day of rest while the chemo in his system continues to clear out all the soldiers from his army bases (including the civilian side of his bone marrow that produces red blood cells). On Day 0 the transplant date, we will infuse Idan with the donor’s army. His army has been found to be a 12/12 match to Idan’s. While this is great news, it is not the whole picture. This new army is not really going to understand how to relate to all of Idan’s body parts, and will most likely still want to attack some of it (this is called Graft ss Host disease, and it happens with 70% of the transplants from unrelated donors like Idan’s). For this reason they use the ATG, and the other immunosuppressants to allow the new army to come into the empty base, but forces it to unpack, train, and start patrolling very very slowly. Giving the new army more time to get adjusted to Idan’s body is a delicate balancing act that will happen over the next year. Since they are letting the bone marrow come in and start working very slowly there is a longer time where Idan is lacking any working immune system and will be kept in isolation as well as be given drugs to protect him.
– So what is next?
Day -6 to day 0 we are clearing his bone marrow and making room. On Day 0 he gets the transplant, and we start counting days until the bone marrow travels to the base and starts setting up shop. We hope to hear around Day 22 that they have reached the base and that would be engraftment. We will then wait until we see his counts go up. The first type of soldier to come back (or, better put, to “grow”) is his neutrophils (which work fine now, but we have to get rid of them with the rest of the army) and they will wait until that level is good enough to get released to isolation at our apartment. This will happen between day 30 and 50 and then we will count to day 100 before they might let us go back to NYC. From then on and until around 2 years post transplant Idan will still have a weak immune system. Our hope is that around one year post-BMT, his new army will be strong enough and acclimated to his body to start reducing the supplemental protections we are giving him. Along the way there are going to be many scary events but we and the medical team will deal with them as they come up.
In a few years, when Idan can go to school, play with other kids, take swimming lessons, play in the park and ride the swings all with the protection of his donor’s army, we will know we did the right thing to ensure Idan has a normal, healthy and happy life.
For more see here: http://www.hyperigm.org/about-hyper-igm-syndrom/
Author: Akiva
Idan's Blog
First Clinic Day:
by Akiva • • 2 Comments
 Today was our first day back at the SCCA clinic to start the process of the various pre-transplant testing . We started with a nurse visit to go over a lot of basics and get our schedule for the next few days. It is very strange to be back here. Everything is the same, including most of the staff that we meet. It is a bit of an awkward balance between the “how nice to see you again” and the “I’m so sorry you had to come back to do this all again!” Overall, it is nice to have familiar faces and people we feel like we know. For Idan, everyone is new. He has no memory of any of these people and cannot understand why they all seem to know him so well.
Today was our first day back at the SCCA clinic to start the process of the various pre-transplant testing . We started with a nurse visit to go over a lot of basics and get our schedule for the next few days. It is very strange to be back here. Everything is the same, including most of the staff that we meet. It is a bit of an awkward balance between the “how nice to see you again” and the “I’m so sorry you had to come back to do this all again!” Overall, it is nice to have familiar faces and people we feel like we know. For Idan, everyone is new. He has no memory of any of these people and cannot understand why they all seem to know him so well.
After the nurse visit, we had Idan’s first round of blood tests of many many to come. He did very well and sat still while they poked him and took 17 vials of blood. Yes, 17 vials of blood! Not bad for his first draw here. They will take a few more before his procedure scheduled for Friday as he was at his max today for how much they are allowed to take.
We have a nice long break for lunch and went to eat outside. We went down to the marina to see the old boats. Idan could care less about the boats and manly enjoyed dragging Amanda around up and down the trails and just jumping around.
Later on, we had our first visit with Idan’s primary care physician who went over all Idan’s history and did a full physical. All went well and Idan was very excited to come back to the SCCA House, the clinic-related hotel we are staying at, so he could go to the play room.
Our schedule for the next couple of days is busy. Tomorrow we have another full day at the clinic, mostly with meetings (social worker, nutritionist and a  90 min consult with the attending to go over the transplant protocol). He also has an EKG in the morning. Friday will be a tough day, as Idan will have a bone marrow aspiration and biopsy at 12 at Seattle Children’s Hospital and will have to fast all morning since he gets anesthesia. So we expect a hungry and cranky child.
90 min consult with the attending to go over the transplant protocol). He also has an EKG in the morning. Friday will be a tough day, as Idan will have a bone marrow aspiration and biopsy at 12 at Seattle Children’s Hospital and will have to fast all morning since he gets anesthesia. So we expect a hungry and cranky child.
At the moment, unless something changes, we have a couple more weeks of testing, and will be admitted to the hospital on July 12th to start chemotherapy conditioning. The transplant itself will occur around July 18th or so. Good news is that we have found an apartment in the same complex we lived last time. We should be moving in there on July 1st, and it will be nice to have a temporary home as opposed to a hotel room. Idan is not as happy as he says “there will not be a play room” in our apartment. Not easy to please!
We will keep you all updated.
Idan's Blog
Smile – Ten Years Brain Tumor Free
by Akiva • • 2 Comments
“Based on the rate of growth and the location of your tumor you have around two years to live.” That was the sad prediction I heard from dozens of physicians in the summer of 2005. From New York to Boston to Los Angeles and Jerusalem, everyone around the world we consulted had a different approach, but they all agreed: The brain tumor was “inoperable.” I was twenty five years old and one year away from graduating Columbia University. I was way too young to die.
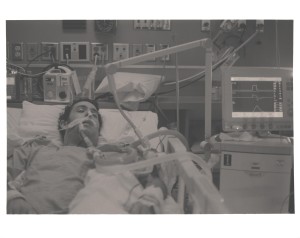 I am still here. Ten years later, I am alive and well and tumor free and the only prediction that came true was the one given by Dr. Robert Spetzler in Phoenix, Arizona. With a big smile on his face he said: “I am 95% confident I can get your whole tumor out, and leave you in not much worse condition than you are now.” At first, it seemed his proclamation might have been an overstatement. On November 8, 2005, Dr. Spetzler successfully remove my whole tumor. While my family was assured the next day that the tumor was all out, and I would be fine, at the time it did not look like it. I was in an induced coma, intubated and had tubes sticking in and out all over my body. I only woke up four days later, when they were finally able to extubate me. I could not feel or move the left side of my body. I could not talk, walk, swallow or do much of anything. The right side of my face was paralyzed and numb, and I could not smile or even hold water in my mouth without it dripping out. Like a newborn baby, I was cradled and tended to by my family and an amazing team of nurses at St. Joseph’s Hospital in Phoenix. Every day Dr. Spetzler came by during rounds, looked at my broken and weak body, and proclaimed, “he is doing great!” Everything will be okay. Eleven days later, I was transferred by plane and wheelchair to NYC to Rusk Rehabilitation Center for what we were told would be a very slow and long process of rehab. There, I learned to walk, talk, swallow and was able to be released to outpatient in three weeks. I continued my rehabilitation out-patient while I resumed classes at Columbia. The right side of my face was paralyzed, and numb, and I had set a personal goal to smile once again.
I am still here. Ten years later, I am alive and well and tumor free and the only prediction that came true was the one given by Dr. Robert Spetzler in Phoenix, Arizona. With a big smile on his face he said: “I am 95% confident I can get your whole tumor out, and leave you in not much worse condition than you are now.” At first, it seemed his proclamation might have been an overstatement. On November 8, 2005, Dr. Spetzler successfully remove my whole tumor. While my family was assured the next day that the tumor was all out, and I would be fine, at the time it did not look like it. I was in an induced coma, intubated and had tubes sticking in and out all over my body. I only woke up four days later, when they were finally able to extubate me. I could not feel or move the left side of my body. I could not talk, walk, swallow or do much of anything. The right side of my face was paralyzed and numb, and I could not smile or even hold water in my mouth without it dripping out. Like a newborn baby, I was cradled and tended to by my family and an amazing team of nurses at St. Joseph’s Hospital in Phoenix. Every day Dr. Spetzler came by during rounds, looked at my broken and weak body, and proclaimed, “he is doing great!” Everything will be okay. Eleven days later, I was transferred by plane and wheelchair to NYC to Rusk Rehabilitation Center for what we were told would be a very slow and long process of rehab. There, I learned to walk, talk, swallow and was able to be released to outpatient in three weeks. I continued my rehabilitation out-patient while I resumed classes at Columbia. The right side of my face was paralyzed, and numb, and I had set a personal goal to smile once again.
 Two years later, in November 2007, I had my diploma from Columbia and went on to obtain an MPH at the Mailman School of Public Health. I was dating the love of my life and was doing great, physically and professionally. But I still could not smile. Sure, I could mostly drink without spilling water out of the side of my mouth, and I had even perfected a method of blowing up balloons. But I had not reached my goal. The cranial nerve that controlled my face was cut or damaged and was not coming back. The doctors had told me over and over again: most deficit improvement is seen in the first 3-6 months. After that, some might still get better in the first 2 years post surgery. But after those two years, things will not improve or come back. My fate was sealed. I may have been reborn as the superhero, iPatchman, but I was destined to always be defeated by DC Comics’ Two-Face.
Two years later, in November 2007, I had my diploma from Columbia and went on to obtain an MPH at the Mailman School of Public Health. I was dating the love of my life and was doing great, physically and professionally. But I still could not smile. Sure, I could mostly drink without spilling water out of the side of my mouth, and I had even perfected a method of blowing up balloons. But I had not reached my goal. The cranial nerve that controlled my face was cut or damaged and was not coming back. The doctors had told me over and over again: most deficit improvement is seen in the first 3-6 months. After that, some might still get better in the first 2 years post surgery. But after those two years, things will not improve or come back. My fate was sealed. I may have been reborn as the superhero, iPatchman, but I was destined to always be defeated by DC Comics’ Two-Face.
Two years later, November 2009, marked some of the happiest days of my life. I just married my true love. I had a dream job in healthcare consulting and life was good. I had outlived all predictions and was tumor free for four years. And despite the utter joy, I could not fully smile. I had perfected the Zoolander Blue Steel look for photos. My wife, Amanda had fallen in love with my half grin and I could not complain. Most people in my situation did not live to tell the tale, and I was complaining about a smile? I continued to refuse offers to surgically stitch my face in a permanent Joker grin and continued my own physical therapy and exercise to keep the little muscle tone I had on my right side of my face.
Two years later, in November 2011, now six years post-brain surgery, I sat at Nonna’s Italian Restaurant on the Upper West Side for my birthday dinner with Amanda. She handed me my birthday present. A little red box with yellow teddy bears. Inside, little baby booties and a handwritten note on tissue paper, with the message “To the greatest love we will ever know.” She was informing me that she was expecting. We were going to have a baby in eight months. Inside, my joy was endless, and yet I still could not smile. Just my regular half grin in response to the best news anyone can get.
Two years later, by November 2013, we had experienced both extremes of any parents’ emotional spectrum. From the new happiest day of my life, the day my son Idan was born, to the scariest and saddest day of our life, the day he was intubated for PCP pneumonia. Even if I wanted to smile, I could not. We were filled of hope now, and longing for a normal life again. Just a few weeks after Idan’s bone marrow transplant, I celebrated my 8th year tumor free. I was full of hope that by my ten-year anniversary Idan would be cured and everything will be back to normal. I stopped believing that I would ever smile fully again, even if I wanted to.
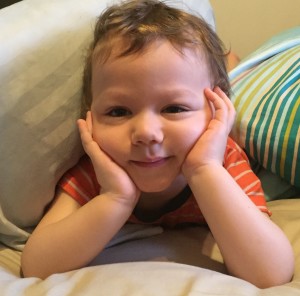
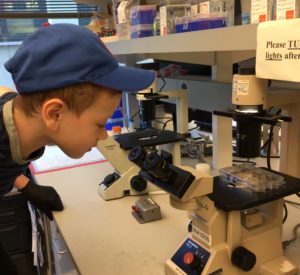
Today, two years later, Idan is not cured. We are heading towards a second bone marrow transplant in the spring, and life might never be normal. But hope is still part of every drop of my being. The same unrelenting perseverance that allowed me to live through an inoperable brain surgery has kept my son alive and well and found him the best care he could receive. My education, life experience and optimism serve me now as the president and co-founder of the Hyper IgM Foundation. Our mission is not only to cure Idan, but to work for a cure for all families and children living with Hyper IgM. I know this can be achieved. I know happiness is possible. I know normality is a state of mind. I know all this because I spend the day smiling. A full smile. I spend the day smiling when Idan wakes up in the morning with a million questions as if the night was just a fleeting moment. I spend the day smiling when I see Idan play with his little cousin and they both laugh uncontrollably. And I spend the day smiling when Idan is solving puzzles way too advanced for his age or building lego sets made for six-year olds.
Sometime, over the last two years of trying to achieve normality in a post transplant world, my smile just appeared. Despite all medical predictions of how or when deficits can recover, I am able to smile with both sides of my face now. Ten years, brain tumor free, and I am smiling every morning when I wake up next to Amanda and when Idan calls us into his room. If my smile can appear again ten years after it was removed along with a tumor that had my name on it, I know that anything is possible. I invite you all to help me make that which is impossible a reality. Help me bring a smile to the families across the world dealing with Hyper IgM Syndrome.
Donate today to my ten year brain-tumor-free fundraising page!
Idan's Blog
Two Years Since The World Turned Upside-down
by Akiva • • 0 Comments
It has been two years since that awful day we rushed our 8 month old son to the ER with an oxygen mask. That April was much warmer than this one, and we had spent much of the time in the two weeks leading up to that day outside in the park and playground. He had just started enjoying the swings and there was always a playground stop after the visits to the pediatrician leading up to that fateful day. I am still amazed by the little boy’s resilience and happy mood. Idan was breathing 80 breaths a minute while the Pneumocystis pneumonia (PCP) was quietly destroying his lungs, but he was as happy as could be and could not wait to play.
It has been two years since we watched our son intubated in the ICU while his lungs gave in to the PCP, not knowing if he would ever recover. We spent three weeks isolated in that room hoping to wake up from a nightmare that was just beginning. We spent three weeks researching PCP survival rates, and immune deficiencies, trying to piece together the mystery of how a healthy happy boy could suddenly fall so ill.
It has been two years since we first heard that words Hyper IGM and CD40 Ligand Deficiency, since our son came back to us and we settled into our isolated life in the center of the busiest island in the world. Our life was changed forever, and our dreams crushed as we faced ever growing uncertainty as to our son’s survival. It has been two years since our baby inspired us to become better people, and gave us the strength to make the hard choices we faced.
It has been two years since our son galvanized thousands of people to open their hearts to our family and form an army of supporters to fight with us. It has been two years since our son empowered us to become experts in his medical condition and gave us the resilience to carry on with our lives. For it is Idan’s resilience, in the face of all that he has endured, that has kept us going all this time.
Your average toddler during this period would learn to walk, talk, play and jump. They would start asking questions and start learning some letters and numbers. They would learn to kick a ball, do puzzles and stack blocks. And they would grow taller and bigger and brighter. It is all a parent can hope and wish for their child during this age.
Idan reached and surpassed all these milestones despite Hyper IGM. He laughs, entertains and sings despite having spent over 65 days in hospital rooms. He learned the ABC’s and his numbers while getting prodded and poked thousands of times. He can put together a 54 piece puzzle of the USA all on his own despite receiving three types of chemotherapy. Nothing has slowed him down or taken away his constant excitement and curiosity, not even the social isolation he has had to endure.
The road ahead is long and rocky. Idan will have to face another transplant, more isolation and many more pokes, meds, and surgeries. It will be more than two years until the cure we hope for him will be in our reach. But despite this, we know that Idan will continue to thrive and develop and inspire us to carry on. He is truly our light and our guide throughout this journey and we will not let him down. Idan is My Hero!
Idan's Blog
One Year Since Our Return to NYC
by Akiva • • 1 Comment
Today marks a year since our return home to New York after Idan’s bone marrow transplant (BMT) in Seattle. It truly is amazing how time flies, and so much can change in our life, yet at the same time still be the same. We left to seattle in September of 2013 full of hope that we would bring home a cured baby and be able to start our normal life again. When we returned to New York last March on day 140 post transplant, we already knew that the cure was slipping away from us.
In those months out in Seattle, the transplant days went by with no major glitches and Idan did well despite the chemo and immunosuppressive treatments. Besides some minor setbacks, it seemed at first that he engrafted and we were sent to outpatient sooner than expected. But as time went by, we learned that the most important part of the donor graft, the T-cell line, never really took hold. We did our best to save it, going back to our generous donor and asking for more cells. In December 2013, we give Idan his first donor lymphocyte infusion (DLI) and waited. By January, we knew that it only gave him a small bump, and unfortunately that small bump came with graft vs host disease (GVHD) of the skin, which required increased immune suppressants and steroids. Throughout this whole time, Idan never really complained and was a happy and inquisitive baby who learned to walk in the halls of Seattle Children’s Hospital and the wonderful outdoors of the Seattle neighborhood we lived in.
When we were allowed to return home last March, we were still full of hope that his graft would take hold and that a cure was still on its way. When we brought Idan back, he was a little toddler full of joy to be reunited with all his family in NYC.
When we returned to New York, our life was so different from the March before. The previous March, before he was diagnosed, we spent our time going to the park, meeting up with our friends with young children, and taking swimming lessons at the JCC. That March, however, passed in isolation, venturing out only for twice-a-week doctor appointments and blood draws. Compared to Seattle, NYC felt like a zombie-filled nightmare with virus spreading strangers at every corner. It was good to be back with family but it was hard to entertain an almost 2 year old boy with this kind of isolation. Idan was on 13 daily medications with 26 different dosages at every time of day and night. Going to his grandparents for the day meant packing ziploc bags with two dozen syringes and planning his nap and meal schedule around the medication times. Idan grew tired of the weekly blood draws and started fighting off the needles. And still, his graft continued to slip away.
In the fall, we returned to Seattle and made one last effort to save the graft with a second DLI. When the graft continued to slip in the weeks and months that followed, it became clear to us that the graft was no longer a graft, and now just a memory – an unfulfilled promise of what could have been.
This past year flew by and we find ourselves a year later very much in the same place we were before leaving to Seattle the first time. Idan has grown up, and turned into a smart, inquisitive and very curious little boy. In July, he will turn 3, but he feels older and wiser for his age (he is also very tall and sturdy, something that is unusual for transplant kids). We are comforted by the fact that he is no longer in post-transplant mode, but he has regressed back to Hyper IGM life. Thankfully, his daily meds consists only of 3 vitamins and supplements and twice a week prophylactic antibiotics to prevent the return of the PCP that landed him in the ICU back in April 2013. Blood draws are infrequent now, and if all goes well, his next draw will only be in May. We still give him weekly infusions on Saturday mornings with antibodies that keep him safe, and he takes those three needle pokes like a real superhero.
Amanda and I have spent the last two years learning everything and anything about Idan’s rare condition. I doubt any doctor or patient out there has read more medical journals on the subject then we have and we continue to try to understand the disease while we asses the risks involved. The facts remain the same though: the median life expectancy is 24 and over 80% of patents don’t make it past their third decade of life. We knew this before transplant and took the high risks then in order for our son to have a long and happy life, and we will do it again in a heart beat.
What this experience has taught us more then anything is that we are goal oriented people, ever focused on our vision of tomorrow, ready to face the challenges along the way.
Ten years ago, when I (Akiva) was diagnosed with a so called “inoperable” brain tumor in my brain stem, I set a goal to be completely cured, regardless of what 30 of the top doctors were saying my chances were. And I met that goal by risking everything and having complicated brain surgery in Arizona with the one doctor in the world that was confident enough to take me on as a patient. Two years ago when Idan was diagnosed, and after the initial shock of the ICU, we set a goal to learn about Hyper IGM and talk to as many experts so we can make the best and most empowered decision on how to cure our son. And we still stand by our decision to uproot our life, leave our jobs, and move to Seattle for six months to cure Idan. Despite the failure of the 1st transplant, we have never given up hope.
We have once again set a goal, to transplant again within the next two years, again in Seattle and with the hope of a better matched donor. Idan will still be under five when we try again, which is the age that the risks of transplant are better controlled.
In the meantime, we continue to live our lives and help Idan thrive and grow. You may have seen the posts on Facebook, as the kid is happy and an extremely energetic two year old. He talks non-stop, expresses his feelings, and loves to learn and build and just have fun. He has always been a happy child, weather in the ICU, getting chemo, tethered to an IV pole or being cooped up in a NY apartment for most of the winter. No matter what, he always wakes up with a smile and declares “Wake up!! Its time to play!”
We would like to thank all of your for your continued support. Idan’s army always has a special place in our heart and it makes us stronger and gives us hope that we can enter again into this battle for a cure and hopefully this time come out triumphant. Someday, in the future, when germs are not the big boogieman anymore, we hope to thank more of you in person for your support.
Idan's Blog
Day 420: It’s Been A Tough Month
by Akiva • • 7 Comments
 It has been two months since our last real blog update. We’ve been updating Idan’s Facebook page more regularly, but it has been a few weeks since we shared any real news. Sadly, it has been a rough few weeks and neither Amanda or I have been in the right place to put it all down in words. I will jump right in then:
It has been two months since our last real blog update. We’ve been updating Idan’s Facebook page more regularly, but it has been a few weeks since we shared any real news. Sadly, it has been a rough few weeks and neither Amanda or I have been in the right place to put it all down in words. I will jump right in then:
We came back from Seattle at the beginning of November (after spending most of October there) with the hope of saving Idan’s failing graft. After putting Idan through more chemo, several long fasting days, dozens of pokes, a PICC line surgery, and a second DLI this October, we checked his chimerism again right before Thanksgiving and did not get good news. The DLI did not work, and his graft is still failing. We were heart broken. We were faced again with the options as before: risk a third DLI or do nothing and start preparing for a second transplant. After many conversations with our Seattle doctors, family and NY doctors we are no closer to making a decision but we have decided to wait for another data point next week to see how fast the donor graft is falling. A third DLI would be at a higher dose, comes with high risk of GVHD, and, given our track record, has a minimal chance of working. A second transplant also comes with more risks than the first one, another long stay in Seattle away from home and our family, and the possibility of rejection.
What has made things harder this month has been the fact that Idan has spent most of the past 4 weeks sick with a cold. Every parent of a toddler dreads when their child is sick, but for us there is always the added stress of being one step away from the ER. Like with a newborn, any fever above 101 or requires doctor visits, blood cultures and a good chance of hospitalization. While Idan can fight a cold virus with the help of the weekly antibodies infusions we give him, any cold can all too easily turn into a pneumonia and we always need to rule out an infection.
Idan has been getting stronger and better at fighting us off when we try to take his blood and there have been way too many blood tests this month. We cannot wait for a time where we can space out these tests and hope and try to keep him safe so that we can avoid unnecessary colds and infections.
The good news is that Idan is still growing, developing and thriving and has an endless amount of energy. He has been talking more every day, and we potty trained him over the Thanksgiving weekend and he has been golden ever since (no pun intended). He has grown an inch and a half since November 1st and he has been developing his art skills along with his imagination.
All we can wish for is a better and healthier 2015 for Idan and the rest of his little Hyper IGM counterparts around the world who inspire us with their bravery and perseverance.
Wishing you all a happy holiday season and a happy and healthy new year!
Idan's Blog
Day 361: A Crazy Week Ahead:
by Akiva • • 1 Comment
So we got our schedule for next week. The good news is that Idan will not be admitted to the hospital except for the day of his DLI and it’s only a day admission so we can most likely go home that night. The bad news is that next week is going to be a living hell for the three of us.
Here is a summary of our week:
Monday: Kidney Test: We have to be at the hospital at 8:00 a.m. for a kidney test. This requires Idan to fast the night before, and he can’t eat any solid foods until after the test is over —- 8 hours later. So for approximately 16 hours, Idan will not have anything to eat. During this time, they will be placing two IVs, one in each arm, and taking blood from one arm while infusing a solution into the other arm. This test is required to measure the dosing of the pentostatin, the chemo drug he will get on Wednesday.
Tuesday: Picc Line: Another day of fasting all day. The only slot available was for 3:00, and Idan cannot eat anything after 7:00 a.m. We have to be at the hospital by 1:45 p.m., and will have to endure over an hour of waiting before the procedure starts.
Wednesday: Chemo infusion at 10:45 a.m.: 5 hours at the clinic during which Idan will receive a continuous infusion of liquids and the chemo will be infused a couple hours into the visit.
Thursday: Break. Whew.
Friday: DLI: We’ll be admitted to the hospital first thing in the morning, Idan will have a couple hours of hydration and then the DLI. After he will be monitored until late in the day/evening. We should be discharged by nighttime.
The following week we’ll have a couple clinic appointments to check for GvH, but they don’t expect to see anything for a couple weeks. He’ll have his picc line removed some time that week (or potentially after the DLI friday, but we have to see how many pokes he has lined up for the following week before we decide when to remove it).
If anyone has any ideas of how to keep a starving two year old who is confined in a room and attached to IVs happy and entertained, we’re all ears.
Idan's Blog
Day 309: Busy Few Weeks
by Akiva • • 0 Comments
 It has been a busy few weeks. At this point in transplant things usually calm down, and doctors visits are more spaced out. For us, less tests and doctor visits would be welcome. Little Idan has had to go in at least twice a week for a visit and a blood test wile we are still trying to adjust his immunosuppressant dosing as well as get him off the steroids. He is on a very low dose of steroids, but his adrenal gland is still not functioning on its own. This means he tests very low when we check his cortisol levels and this can be dangerous if he gets sick or is in an accident. The doctors say it will take time for the adrenal gland to wake up and to be patient. Until then Idan will keep braving the needles and being an amazing sport during doctor visits.
It has been a busy few weeks. At this point in transplant things usually calm down, and doctors visits are more spaced out. For us, less tests and doctor visits would be welcome. Little Idan has had to go in at least twice a week for a visit and a blood test wile we are still trying to adjust his immunosuppressant dosing as well as get him off the steroids. He is on a very low dose of steroids, but his adrenal gland is still not functioning on its own. This means he tests very low when we check his cortisol levels and this can be dangerous if he gets sick or is in an accident. The doctors say it will take time for the adrenal gland to wake up and to be patient. Until then Idan will keep braving the needles and being an amazing sport during doctor visits.
One thing that is never really discussed with all the difficulties of transplant is the crazy amount of medications one is on for a long period of time. Besides the weekly infusions of antibodies, most of the months post-transplant Idan was taking between 9-11 different oral meds each day at 6-7 different time points throughout the day and night. Some days I counted 26 different oral syringes. Now Idan has been truly amazing with taking his meds, and we were lucky to not need a feeding tube during transplant, so he always took his meds orally. In the past month, we have been focused on cutting out the ones we can. We were able to cut out one of the two blood pressure meds he was on. Steroids are almost done, so that means we were able to cut out the antifungal he was on as well. Idan’s swallowing has much improved since we took him off the bottle (no pun intended) and he has been drinking exclusively with a straw for the past few weeks. This means we can cut out the liquid thickeners he was on as well as the acid reflex med. It feels really great to wake up on some mornings and only have to prepare 5 meds with his breakfast. Realizing that most parents probably dread giving their kids one medication, I think we are in a good place.
Our next big journey coming up is our return to Seattle for Idan’s one-year follow-up visit. We have started telling Idan that we are taking a trip to Seattle and will be going on a plane. Oddly, he keeps saying “home?” whenever we mention our trip to Seattle, so I guess he still has some memory of his time there. Nothing wrong with being a bi-coastal baby I guess.
Facebook, Idan's Blog
Idan Has a Cold & Strange Our Strange 5 Year Anniversary
by Akiva • • 0 Comments
Today was a strange day. It’s was our 5 year anniversary and Idan went over to Amanda’s family for an “adventure”. Like every Saturday, the day started off with Idan’s SubQ IGG infusions and a nice bowl of cereal then Idan’s grandfather picked him up and Amanda and I went downtown for a lovely brunch (turns out Amanda and I have not taken the subway together in over 16 months!). After brunch, Idan, who had woken up with the sniffles started to run a slight fever, so we came back up to Amanda’s family to be with him. It’s a tricky week for him to get a cold as we are trying to get him off steroids but his own system is still not making enough cortisol. By dinner time he had a fever and we started to worry that we might need to go to ER. We spoke to our amazing pediatrician who takes our calls on weekends, and decided to wait to see how he is in the morning. We canceled out dinner plans and babysitter (my brother) and Idan ended the day getting cheered up with a new dish set toy he got for his birthday. Currently he is already sound asleep while I write this post. We lead a strange life. There is no rest for the weary. Hope tomorrow he is feeling better.
From Facebook:
Idan's Blog
Day 243: It’s been that kind of a month.
by Akiva • • 3 Comments
 Wow, I cannot believe it has been a whole month since our last blog post. Sorry to have been away so long. I know we post small updates on Facebook, but that is never enough to keep our friends and family really updated. It has been a very busy month and I am going to try to make sure I cover the important parts:
Wow, I cannot believe it has been a whole month since our last blog post. Sorry to have been away so long. I know we post small updates on Facebook, but that is never enough to keep our friends and family really updated. It has been a very busy month and I am going to try to make sure I cover the important parts:
Idan had his first cold in over a year:
This was the scariest part of the month and had us very close to being admitted to the ER. Two weeks ago, on a Monday morning, Idan woke up with what appeared to be a cold. Now, post transplant patients like Idan receive regular infusions of IgG’s (antibodies), which can help Idan clear a common cold and certain viruses, but it can nonetheless quickly turn into a nightmare. Seattle was most concerned about the risk of this turning into a chest cold or pneumonia which Idan would have a much harder time clearing. Idan was running warm and the rule from our immunologist in NYC was that if he hits 100.4 we need to go straight to the ER. We had Idan’s immunologist confer with and prep the bone marrow team at Columbia to see what protocol they had and if we could bypass the ER (which is a germ infested place). Amanda stayed home from work as Idan’s temperature rose to 100 and it looked like we would be going in. As the day went on and Idan’s temperature hovered around the 100 mark, Seattle said they wanted us to go to the doctor to have a virus test done to know what we were dealing with. Thankfully, the fever went down the next morning, and the test results came back shortly after confirming he had the Rhinovirus, a.k.a. the “common cold,” and upped the temperature threshold for going to the hospital to 101F (which he never reached).
All in all it was a scary few days of feeling that we might be admitted any day (last time we were admitted in Seattle for a fever of 100.4 we had to stay for 8 days), and poor little Idan had been suffering with sneezes and a very runny nose. The strangest part about it all is that, because Idan has a Primary Immune Deficiency and has recently underwent transplant, we have been keeping him so safe and healthy that this was his first cold since the PCP last April! Luckily, by the end of the week, Idan’s cold symptoms went away and we were all able to relax a bit.
New Chimerism Results:
Last Monday we sent Idan’s blood to Seattle again and got the result on Friday. Once again very confusing results. As you may recall, last month we were upset to see his donor T-Cells drop from 30% to 15%, and this month they shot back up to 32%. This is very strange behavior and no one really knows what to make of it. Sadly, while last time his Myeliod cells held tight at 20% they have not dropped down to 13%. What this all means is still not known, except we do know that Idan’s donor graft is struggling, and may ultimately fail. But we are holding on tight to our sliver of hope that, if he can hold on to that 32% of donor t-cells, he has a chance at a cure and we would not need to transplant again. So we are still praying and hoping it sticks. Nothing changing with any of his treatment course, and we still hope we can get him off the steroids for the GVHD in the next month or so.
Moving, growing, thriving:
 The other big news of the month, and what has kept us very busy is that we moved apartments last week. Since Idan got sick we knew we would need a larger place for him to grow and run around in. A one bedroom is okay for a baby, but not for an active toddler that can’t go to the playground and spends most of the day at home. Luckily, a larger 2 bedroom apartment opened up in our building and we did not have to move very far. Idan is loving the new place. We painted his room colors he chose and he runs around playing hide and go seek and enjoys exploring all the nooks and crannies (still unpacking so there are a lot of them). Idan has also been talking more, putting together sentences and thriving like most boys his age. We are extremely grateful that he has not missed a beat even with all the medical care and constant medical treatments he has to endure.
The other big news of the month, and what has kept us very busy is that we moved apartments last week. Since Idan got sick we knew we would need a larger place for him to grow and run around in. A one bedroom is okay for a baby, but not for an active toddler that can’t go to the playground and spends most of the day at home. Luckily, a larger 2 bedroom apartment opened up in our building and we did not have to move very far. Idan is loving the new place. We painted his room colors he chose and he runs around playing hide and go seek and enjoys exploring all the nooks and crannies (still unpacking so there are a lot of them). Idan has also been talking more, putting together sentences and thriving like most boys his age. We are extremely grateful that he has not missed a beat even with all the medical care and constant medical treatments he has to endure.
Next month Idan is turning two and we are very excited (and unbelievably fortunate and blessed) to be able to throw this incredible little boy an intimate birthday celebration for him with close family in our new home.
Hope we can update again soon. Make sure to follow Idan on Facebook.